This #OTalk will be hosted by @smileyfacehalo and @preston_jenny
Learning styles (Kolb et al, 1984) have traditionally been considered as a key construct particularly in the preparation of students for practice education. Traditionally students and practice educators have completed questionnaires to help identify their preferred learning styles with the ambition of incorporating these preferences within the learning experience and in some cases even matching practice educators and students on their preferences. This process led to an understanding that we each learn differently and therefore require different learning experiences.
Advances in theory and evidence are now challenging these perspectives to the extent that some theorists believe that learning styles are nothing more than an imaginary fallacy and do not exist (https://www.youtube.com/watch?v=855Now8h5Rs). This may feel contentious and challenge the familiar yet there is a need for us to consider alternative perspectives to ensure that we co-create the best learning opportunities for our future workforce.
During this chat we would like to explore the concept of learning preferences and what this means for students particularly in preparation for placements through the following questions:
1. Are we still teaching students about learning styles and are we still asking students about their preferred learning styles on placement?
2. Does this pigeon-hole students into one learning style?
3. Do you use any other mechanisms to talk about and understand student learning preferences?
4. What might practice educators ask students, and what information should students bring to placement about their learning preferences and needs?
5. How do you incorporate this within the learning experience?
6. What changes are required within the profession to enable an approach that focuses on learning needs and preferences instead of learning styles?
References
Kolb, D. A., Rubin, I. M., & McIntyre, J. M. (1984). Organizational psychology: readings on human behavior in organizations. Englewood Cliffs, NJ: Prentice-Hall
POST CHAT
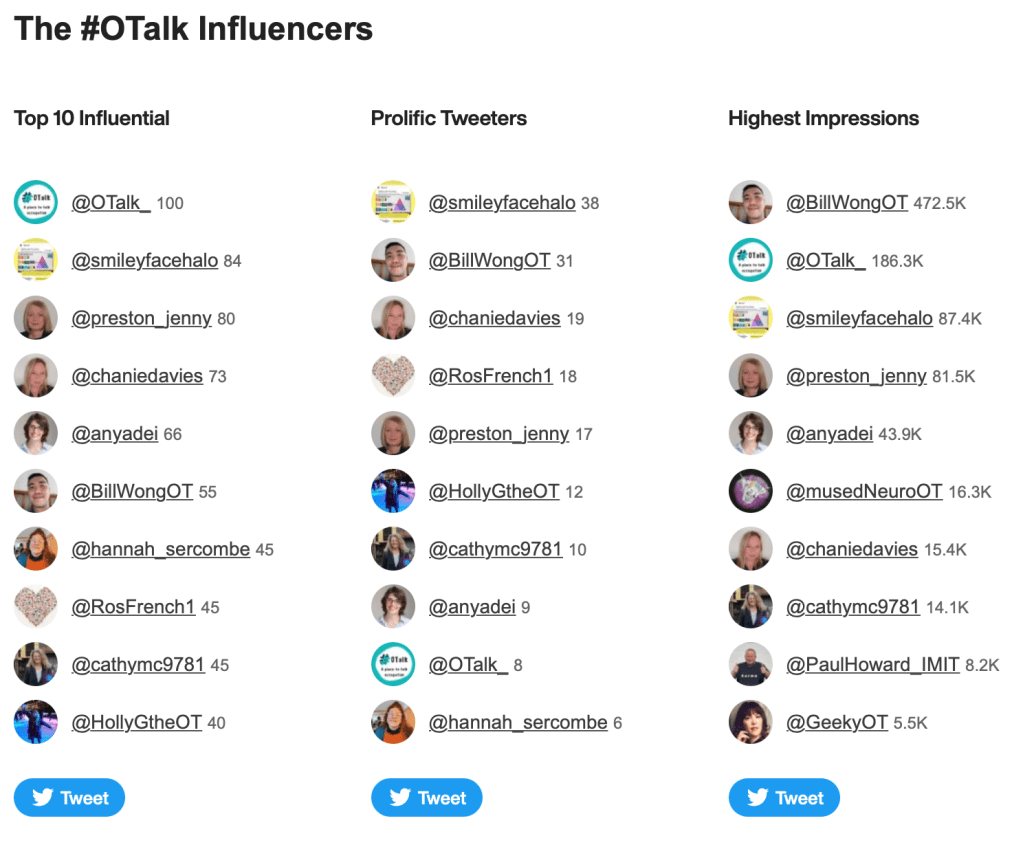
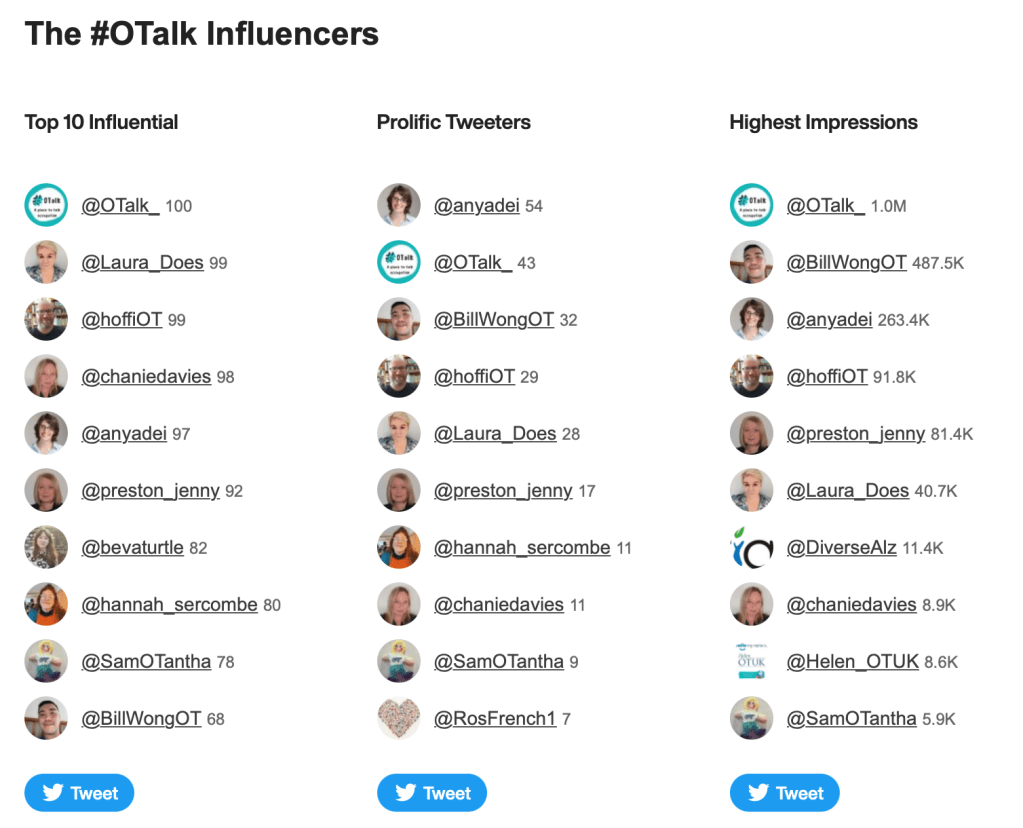
Host: @smileyfacehalo and @preston_jenny
Support on OTalk Account: @smileyfacehalo and @preston_jenny
Evidence your CPD. If you joined in this chat you can download the below transcript as evidence for your CPD, but remember the HCPC are interested in what you have learnt. So why not complete one of our reflection logs to evidence your learning?
HCPC Standards for CPD.
- Maintain a continuous, up-to-date and accurate record of their CPD activities.
- Demonstrate that their CPD activities are a mixture of learning activities relevant to current or future practice.
- Seek to ensure that their CPD has contributed to the quality of their practice and service delivery.
- Seek to ensure that their CPD benefits the service user.
- Upon request, present a written profile (which must be their own work and supported by evidence) explaining how they have met the Standards for CPD.