This week #OTalk is hosted by Jon Fisher @fisheraddiction, here is what he has to say. If your new to OTalk find out here how to join in live on twitter every Tuesday 8pm Supported by Carolina.
The inclusion of occupational therapy intervention for people with addiction first appeared in the 1950’s in the ‘Clinical trial of occupational therapy in the treatment of alcohol addiction’ (Hossack, 1952). More recently, the concept of ‘addiction as occupation’ has been explored more thoroughly by Wasmuth, Crabtree & Scott (2014). They argued that by framing addiction through an occupational perspective, it can highlight barriers to recovery and treatment retention. This in turn could form the basis of occupation-focused intervention as a novel perspective in contemporary treatment services.
‘By acknowledging addiction as an occupation and then focusing on this occupation’s gains and harms, occupational therapists may be in a position to gain trust of clients and help them to make adjustments to their occupational lives that are personally beneficial.’ (Wasmuth, Crabtree & Scott, 2014).
The professional assumption is that engagement in meaningful occupation promotes health and wellbeing (Yerxa, 1998). However, Twinley (2021) has argued the need to ‘illuminate the dark side of occupation’, challenging this assumption that all engagement is healthy. Twinley argues that by fully exploring the individual meaning behind occupations that can also be detrimental to health, we can gain new insights and move closer to truly holistic care.
In a scoping review, the most commonly described interventions included those that promote leisure; included skills training to facilitate activities of daily living; vocation based and those aimed at re-establishing community based sober routines (Ryan & Boland, 2021). It is by fostering a sense of competence through occupational participant that Patel, Scott and Bradshaw (2021) argue is the distinct value occupational therapy brings to promoting lasting recovery and reducing harm.
With the UK’s ageing population (ONS, 2020) and an increasingly complex service landscape, evidence has shown it is the ageing ‘baby boomer’ generation who are at increasing risk from alcohol use. By drinking at the same level in their 40’s and beyond, this increases the risk of the harms associated with alcohol (Drink Wise, Age Well, 2021). Alcohol Related Brain Damage (ARBD) is increasingly recognised in services, with those in their 40’s and 50’s as the higher risk group (Royal College of Psychiatry, 2014). Changes in functional abilities arising from altered cognition fall well within the domain of occupational therapy with compensatory or rehabilitative interventions that promote occupational performance.
Careful consideration is encouraged when addressing substance use in older adults (Royal College of Psychiatrists, 2018) in what ‘Our Invisible Addicts’ report describes as a ‘constellation of risks’. It argues for similar interpretation of risks and benefits of and individuals substance use on their physical and mental wellbeing; something that the concept of ‘addiction as occupation’ can support.
There is a shortage of research concerning neurodiversity and substance use. Addictions UK (2020) found in their literature review that the studies available tended to focus on adult males who have had contact with the criminal justice system. The National Autistic Society (2022) describes how someone with autism may use or become reliant on substances due to the stress arising from masking in order to ‘fit in’. They make a series of recommendations to ensure services are accessible. It is clear further understanding and changes are needed across the board.
In order to promote practice in this area and foster joint understanding, The Occupational Therapy and Substance Misuse Network has formed covering the UK and Ireland. The network has linked with over 30 occupational therapists working in substance use and related services. These include a diverse range of settings including specialist community services, inpatient detox and residential rehabilitation, homelessness, adult social care, community and liaison mental health services encompassing NHS, local authority and private sector services.
QUESTIONS FOR OTALK:
- What brings you to OTalk about occupational therapy in substance use?
- What value does the occupational therapy role bring to substance use settings?
- Outside of specialist substance use services, where do occupational therapists come into contact with service users experiencing substance and addiction related harms?
- What role can occupational therapists play in tackling stigma associated with substance use and addiction?
- How can occupational therapy ensure that substance use services/treatment is accessible to everyone?
REFERENCES:
Addictions UK (2020) Towards better and more joined up policy & practice for people with addictions & neurodiversity conditions Our journey so far… Available from: Towards better and more joined up policy & practice for people with addictions & neurodiversity conditions (addictionsnortheast.com)
Amorelli, C.R. (2016). Psychosocial Occupational Therapy Interventions for Substance-Use Disorders: A Narrative Review. Occupational Therapy in Mental Health, 32(2), pp.167–184
Drink Wise, Age Well (2021) 2015 – 2021: Evaluation of the Drink Wise, Age Well programme. Availabel online: evaluation-report-2015-2020.pdf (drinkwiseagewell.org.uk)
Hossack, J. R (1952) Clinical trial of occupational therapy in the treatment of alcohol addiction. American Journal of Occupational Therapy. 6(6): 265-6.
National Autistic Society (2021) Addiction. Available online: Addiction (autism.org.uk)
Patel, R., Scott, S.L. and Bradshaw, M. (2021). Individuals With Substance-Related Disorders: Lived Experiences and Perceptions of Daily Life. The American Journal of Occupational Therapy, 75(Supplement_2), p.7512510233p1-7512510233p1.
Rojo-Mota, G., Pedrero-Pérez, E.J. and Huertas-Hoyas, E. (2017). Systematic Review of Occupational Therapy in the Treatment of Addiction: Models, Practice, and Qualitative and Quantitative Research. American Journal of Occupational Therapy, [online] 71(5), p.7105100030p1. Available at: https://ajot.aota.org/article.aspx?articleid=2646442
Royal College of Psychiatrists (2018) Our Invisible Addict. Available from: Our Invisible Addicts (2nd edition, CR211 Mar 2018) (rcpsych.ac.uk)
Royal College of Psychiatrist (2014) Alcohol and brain damage in adults: With reference to high risk groups. Available online: college-report-cr185.pdf (rcpsych.ac.uk)
Twinley, R. (2021). Illuminating the dark side of occupation : international perspectives from occupational therapy and occupational science. Abingdon, Oxon ; New York, Ny: Routledge.
Yerxa, E.J. (1998). Health and the Human Spirit for Occupation. American Journal of Occupational Therapy, 52(6), pp.412–418. doi:10.5014/ajot.52.6.412.
POST CHAT
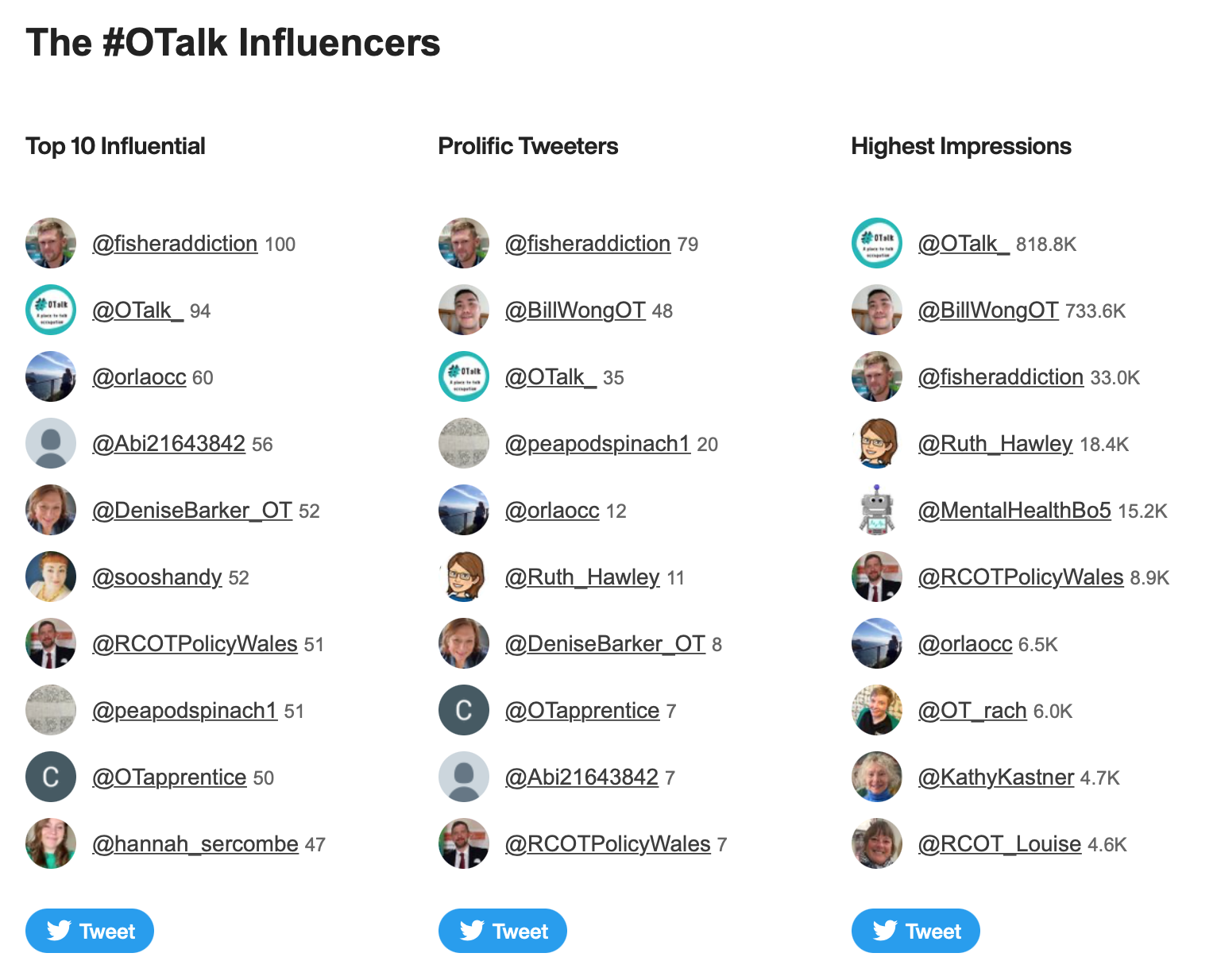
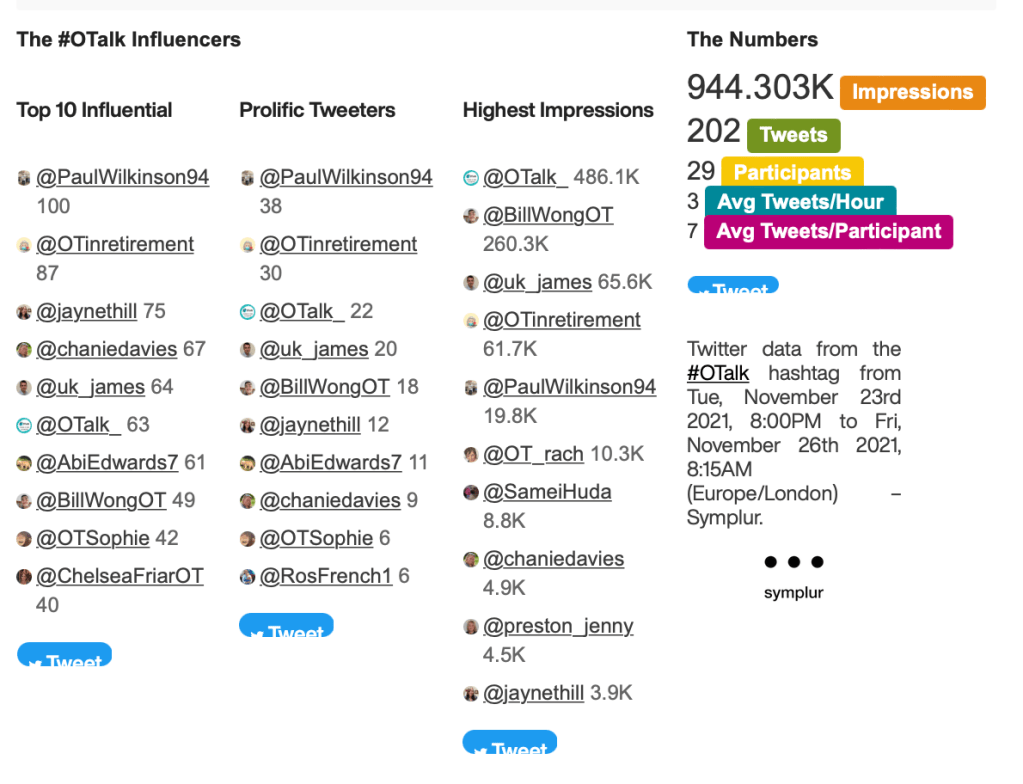
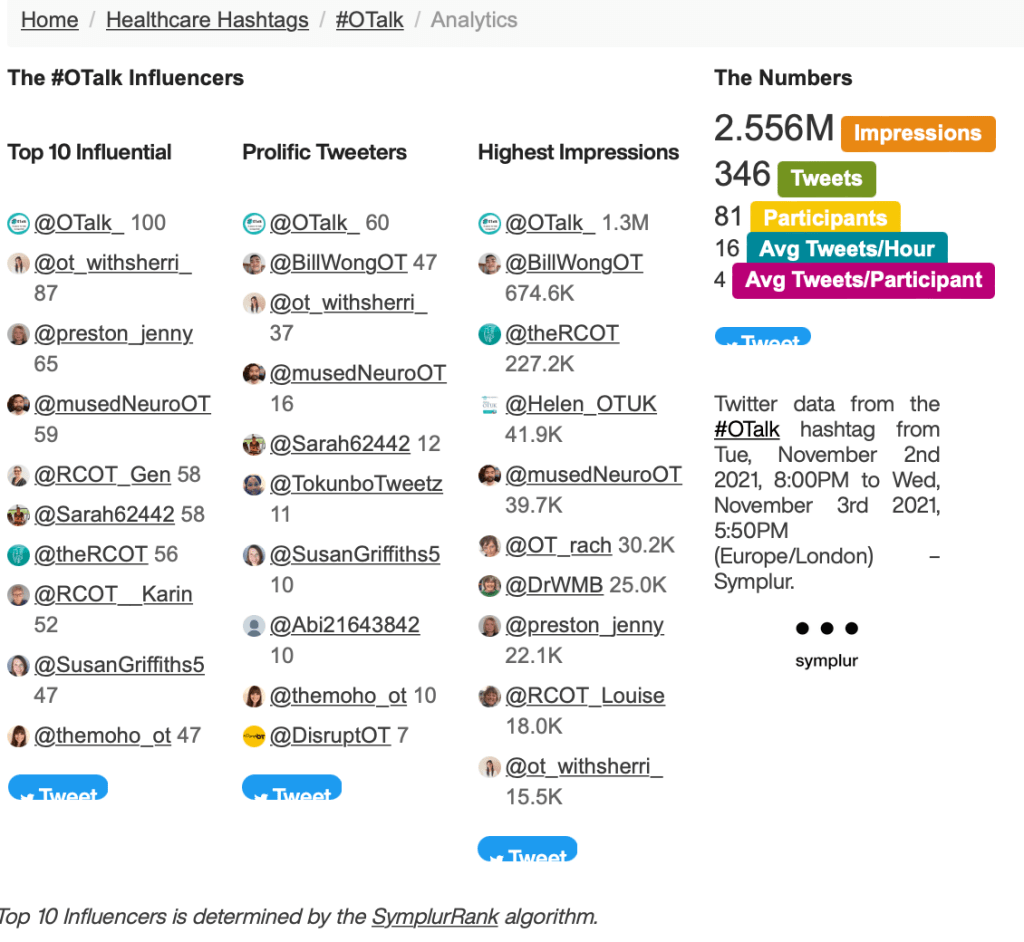
Host: Jon Fisher @fisheraddiction
Support on OTalk Account: Carolina.
Evidence your CPD. If you joined in this chat you can download the below transcript as evidence for your CPD, but remember the HCPC are interested in what you have learnt. So why not complete one of our reflection logs to evidence your learning?
HCPC Standards for CPD.
- Maintain a continuous, up-to-date and accurate record of their CPD activities.
- Demonstrate that their CPD activities are a mixture of learning activities relevant to current or future practice.
- Seek to ensure that their CPD has contributed to the quality of their practice and service delivery.
- Seek to ensure that their CPD benefits the service user.
- Upon request, present a written profile (which must be their own work and supported by evidence) explaining how they have met the Standards for CPD.