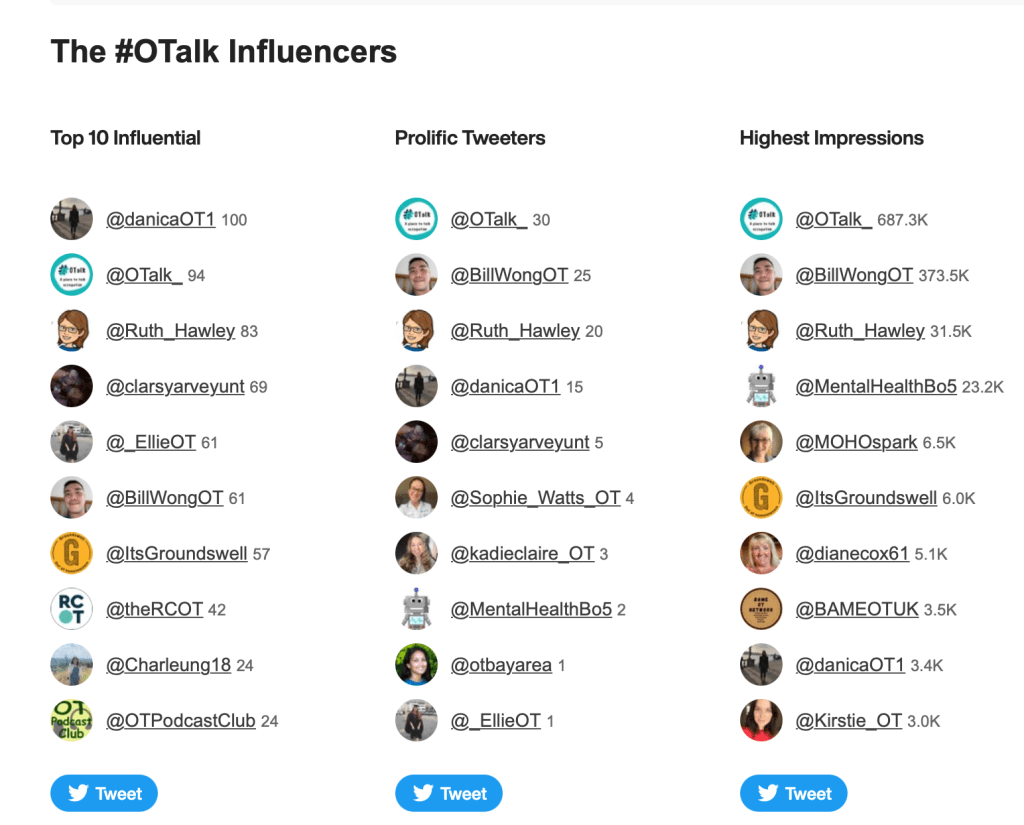
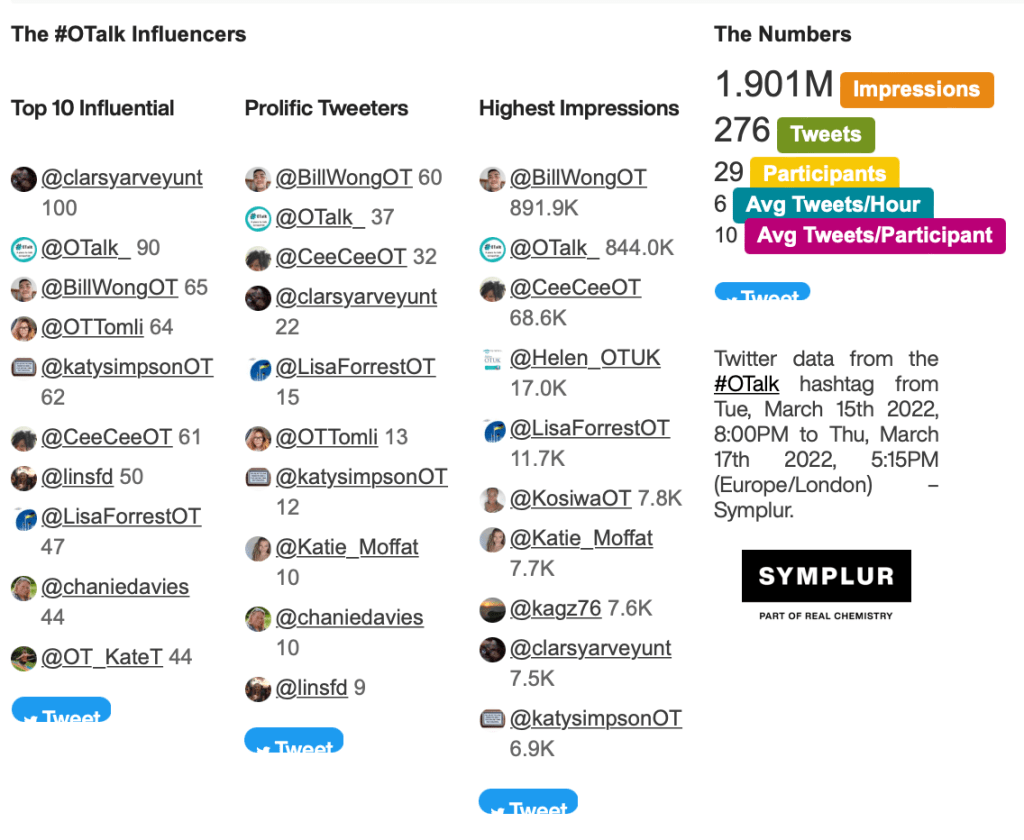
This chat will be hosted by Danica Moller (@DanicaOT1) with Carolina Cordero (@colourful_OT) supporting from the @OTalk_ account.
Danica is an occupational therapist working in a rough sleeper mental health team, in London. Through OTalk tonight, she aims to explore the role of occupational therapy when working with people who are sleeping rough.
Statistics regarding people who are sleeping rough, in the United Kingdom clearly indicate severe health inequalities and much poorer health outcomes. People who sleep rough over a long period of time face a higher likelihood of dying prematurely, with the average life expectancy of a rough sleeper in the UK being 44 years for a male and 42 years for a female (Health matters: rough sleeping, 2022; Office for National Statistics, 2022). Many who sleep rough have co-occurring mental ill health and substance misuse needs, physical health needs and have experienced and continue to experience, significant trauma (Health matters: rough sleeping, 2022).
There is often a view that the solution to the numbers of people sleeping rough, is just having better access to housing. Whilst this can certainly be the case for some, there is a population of people sleeping rough whose mental health has not only been a contributing factor to their circumstances but also a barrier to getting back into appropriate accommodation. This is further challenged by what an individual faces in trying to access appropriate mental health assessment, treatment and care. This could be to do with services not being set up adequately, prejudice and assumptions that are made about them, and also strict inclusion criteria (Health matters: rough sleeping, 2022). This could also include barriers that result from an individual’s cognitive and physical health, financial hardship, lack of awareness and understanding of the impact of mental health on their wellbeing or environmental restrictions such as lack of suitable transport and location (Baker and Jones, 2021). If the individual experiences substance dependence, as a high portion of people sleeping rough do, then the barriers to accessing services are even greater (Health matters: rough sleeping, 2022).
So considering that occupational therapists are trained to explore and address both physical and mental health, what is the role for an OT within this population? Are we as a profession doing enough to support, address and advocate for the needs of rough sleepers?
To explore this topic, tonight we will discuss the following questions:
- Do you have experience working as an OT with rough sleepers? What can OT offer to people sleeping rough who present with mental health needs?
- What are the barriers someone who is sleeping rough faces trying to access mental health care? How can services better support engagement?
- What are examples of occupational injustice that someone who is rough sleeping faces?
- What standardised or non-standardised occupational therapy assessments could be used to gain an understanding of functional difficulties an individual sleeping rough faces? Consider some of the creative ways an OT could work to try and complete a thorough OT assessment, without having access to a standard ‘home’ or ‘hospital’ environment?
References
‘Good work being undone’: 11,000 people slept rough in London during Covid-19. The Big Issue. (2022). Retrieved 9 March 2022, from https://www.bigissue.com/news/housing/good-work-is-being-undone-11000-people-rough-sleeping-in-london-in-covid-19/.
Baker, H., & Jones, G. (2021). Helping homeless people to reclaim and rebuild their lives. OTnews, (29(12), 18-21.
Deaths of homeless people in England and Wales – Office for National Statistics. Ons.gov.uk. (2022). Retrieved 6 March 2022, from https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsofhomelesspeopleinenglandandwales/2019registrations#:~:text=The%20mean%20age%20at%20death%20for%20the%20identified%20homeless%20deaths,years%20and%2062.4%20years%20respectively.Health matters: rough sleeping. GOV.UK. (2022). Retrieved 12 March 2022, from https://www.gov.uk/government/publications/health-matters-rough-sleeping/health-matters-rough-sleeping
POST CHAT
Host: Danica Moller (@DanicaOT1)
Support on OTalk Account: Carolina Cordero (@colourful_OT)
Evidence your CPD. If you joined in this chat you can download the below transcript as evidence for your CPD, but remember the HCPC are interested in what you have learnt. So why not complete one of our reflection logs to evidence your learning?
HCPC Standards for CPD.
- Maintain a continuous, up-to-date and accurate record of their CPD activities.
- Demonstrate that their CPD activities are a mixture of learning activities relevant to current or future practice.
- Seek to ensure that their CPD has contributed to the quality of their practice and service delivery.
- Seek to ensure that their CPD benefits the service user.
- Upon request, present a written profile (which must be their own work and supported by evidence) explaining how they have met the Standards for CPD.