Chat will be hosted by @preston_jenny
Despite the abundance of evidence in existence finding answers to our clinical questions can remain challenging. Whether you are seeking to explore the evidence base or develop an idea for further research, the one thing that is key to everything is the ability to formulate a clear and specific question. In this #OTalk I want to take you on a journey from that early curiosity through to publication of new and emerging evidence.
My journey started 9 years ago when I was given responsibility for setting up a service for young people living with a neurological condition as they transitioned from child health to adult services. As a clinician it felt like a fairly natural thing to do. After all I had many years of clinical experience so why should this be any different? And there the questions began … I had spent a career working with adults living with neurological conditions so what did I know about young people and their needs? What did I know about transition? How might I be able to help them? What would a service need to look like? How will I know if it is helpful? What interventions will I need to offer? What about the legislation? What is everyone else doing?
As a busy clinician I didn’t necessarily have the time to commit to additional study or even time to review the evidence so like many I just started doing what “felt right.” Yet I remained curious, fuelled by my observations that I was being asked different questions; that I was delivering different interventions; and that the more engaged I became the less I seemed to understand the concept of transitioning. There seemed to be so many questions at this stage and even when I did engage with the evidence I didn’t really know what I was looking for as on reflection I had not yet formulated my questions. I really did not know where to start.
However after some reading I started to formulate my thoughts into three main categories as follows (McCombes, 2022, http://scribbr.co.uk):
- Describing and exploring:
- What are the characteristics of this population?
- How do their needs change over time?
- What causes this change?
- How is this dealt with?
- Explaining and testing
- What are the trends/relationships within/between this population and any other group?
- What is the role of occupational therapy within transitions?
- What is the impact of occupational therapy?
- Evaluating and acting
- What are the advantages and disadvantages of interventions?
- How effective are interventions?
- How can interventions be improved?
Suddenly it became much clearer to me as I realised that there were many questions that required to be answered and each with very different purposes. This structure enabled a more focussed approach to a single topic. It helped to clarify that there was not one single question but this would in fact become a series of questions, all designed around a single topic that should aim to improve understanding rather than demand a ready-made solution (McCombes, 2022, http://scribbr.co.uk).
We have subsequently developed three studies based on this programme of enquiry:
- An overview of interventions used across the life span to support transitions of those with a neurological condition: a systematic review of reviews
- A qualitative evaluation of transition experiences from individuals living with a neurological condition
- Exploring the clinical interventions within a Transitions Programme through the use of the ICF
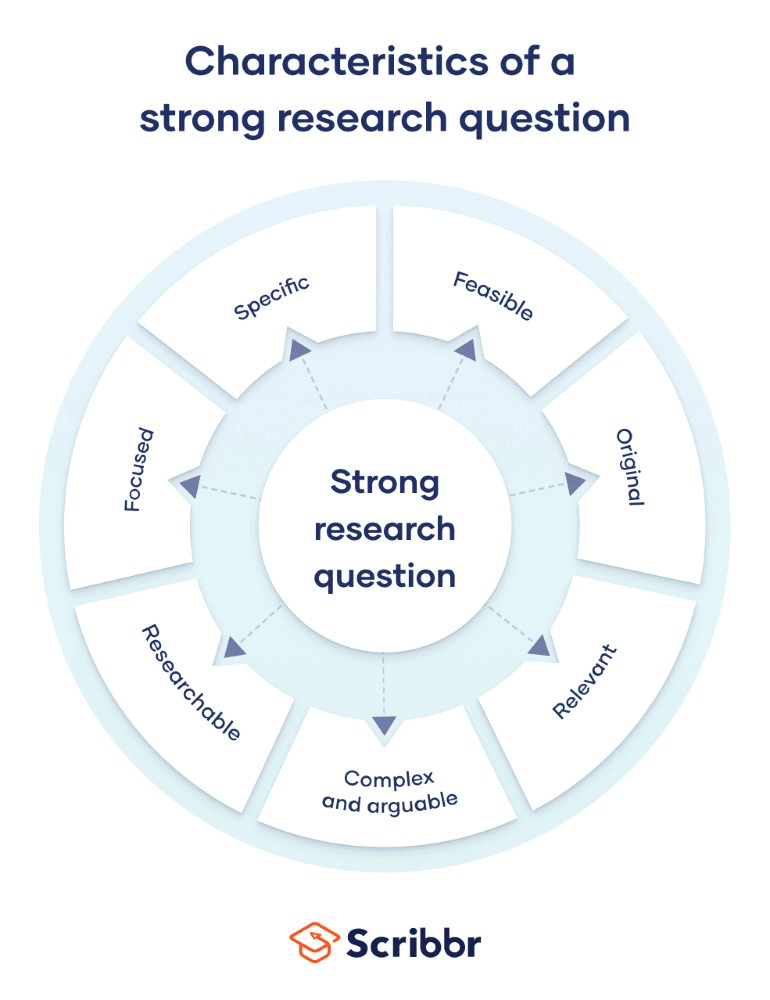
These studies are all at various stages of development and are being prepared for publication with one already accepted. The main learning throughout this journey has undoubtedly been around the following key principles (adapted from http://scribbr.co.uk):
- Focussing on a single problem or issue
- Researching using primary and secondary sources with a clear question in mind
- Feasible to answer within time constraints and practical constraints
- Specific enough to answer thoroughly
- Complex enough to develop the answer into a meaningful presentation, paper or publication
- Relevant to your area of interest (clinical or research)
Tonight’s chat will focus on the following key questions:
- Have you ever had to develop a research question?
- What resources did you access to help?
- How did this meet your needs?
- Were there any limitations?
- What advice would you give to anyone writing a research question?
