For the Last #OTalk of 2021, we have @OT_Expert hosting here is what they had to say….. Join us 8pm on twitter check out our guild explaining how to join in if you’re unsure.
Health and social care practitioners are typically vocational in their work, prioritising high quality person-centred care and support, helping the client acquire skills they need for life. We often find ourselves advocating for our clients to receive necessary support, services and accommodations so that they can achieve their own goals. While much of our practice is based on the Social Model of Disability, focusing on strengths and seeking environmental adjustments to accommodate an individual’s disability needs, the Medical Model also dominates much of our clinical thinking and approaches, often determining who we help or don’t help and how we help our clients.
Medical Model practices include a focus on diagnosis and cure, treatment, identifying impairments and deficits/disorders, and defining how much someone deviates from the ‘norm’. We look to medical model handbooks of disease and disorder (i.e. DSM-5 and ICD-10/ICD 11) to describe a human-being whose psychology, adaptive behaviour and communication diverges from what is the currently constructed normal. These manuals immediately condemn neurodivergent people to being defined as abnormal and disordered, in need of treatment for essentially just being themselves e.g., Autism Spectrum Disorder, Attention Deficit Hyperactivity Disorder. Particularly, in the context of Autism, the focus on treatment and cure has fuelled the Autism Industrial Complex (Broderick, 2017; Broderick & Roscigno, 2019), a billion dollar industry that profits on people’s ableist fears and stigmatising, false autism narratives.
With the growth in understanding of Neurodiversity over the last three decades, there is a dawning realisation that our knowledge and professional training, which has been significantly informed by the Medical Model and neuronormativity, falls short when we contemplate how to provide support for neurominority clients such as our Autistic, ADHD, and dyspraxic clients and those with acquired neurodivergence such as those with mental health conditions and trauma. The expressed views of Neurodivergent clients, the Autistic community, Autistic researchers and advocates call for us to reflect on our practices and the systems in which we work and consider if we need to fundamentally change how we view our clients, the language we use about them, and the assessments and ‘treatment’ programmes and protocols used. There could be a benefit for all, not just neurodivergent populations. This could lead us to not just be person-centred, but person-led. Rather than looking to standardised testing, we look to what a person needs and wants, to be able to achieve their self-chosen goals.
To begin reflecting on what we might need to do to change, improve or consolidate our practice, we need to understand how we got here first:
Since the concept of norming was born in the mid-1800s, the healthy has been separated out from the unhealthy. Over time, norms for human development, language, communication and social interaction have constructed what it is to be “within normal limits” and those outside of these stated norms are described as deficient, abnormal, atypical, unusual, with inappropriate behaviour, for example. This norming centres society’s mind, the mind of researchers, educators and clinicians on seeing neurotypicality as something that must be obtained to have a good, fulfilling and productive life. Those outside the norms are judged as less, talked about as a burden, are pushed to “try harder”, to develop resilience, to strive to reach the centre-ground normalcy, to suppress their ‘atypical’ coping skills so they won’t get bullied and to adopt neurotypical social skills so they can live in the “real world.” Here, we have the seeds of ableism which oppresses marginalised neurominorities.
The Oxford dictionary defines Ableism as “Discrimination against people who are not able-bodied, or an assumption that it is necessary to cater only for able-bodied people.” Ableism is a system of thinking and doing that actually harms disabled people. Ableism is endemic in health and social care seen, for example, the use of standardised testing, norming, neuronormative therapy goals, fluent speech being seen as preferable to stammering or not being able to speak clearly or at all, eye contact and joint attention goals, social skills training, goals to tolerate sensory distress for other’s comfort, those with hyperacusis being advised to not become dependent on noise-cancelling headphones, fading of disability supports to achieve ‘independence’, and disabled teens/adults being discouraged from using support objects that are seen as ‘childish’. Ultimately, behaviourally-based, medical model therapy supports result in the disabled person being denied the support that they actually need as well as being denied opportunity to develop authentically, conditioned and pushed towards a neurotypical ‘normal’ performance.
This sets the individual up for a life-time of unmet needs, trauma from being misunderstood, being gaslit, and having their concerns and discomfort dismissed. Self-esteem difficulties and poor mental health are an all too common side effect of treatment in the Medical Model. We cannot be concerned about the mental health and suicidality of autistic people, if we are at the same time supporting therapies that feed into their mental ill-health.
Regarding accessing mental health services, a common complaint of Autistic people is of being denied access to services because they are Autistic. This happens in both children and adults’ mental health services where those experiencing psychological distress are explicitly denied access to support services, on the basis that the problems they are experiencing are “just part of being autistic”. Failures to understand autistic experience, autistic perception and processing, leads to other access barriers or mis-diagnosis in physical health services. Autistic people and those with psychological distress can often be described as “attention-seeking” “manipulative” “hypochondriac” and their symptoms are not believed (e.g. differences in pain perception – very high or very low thresholds, sensory processing differences.).
Much of our health systems do not provide accessible ways for disabled and neurodivergent clients to engage in services. Additional time may not be provided in session to account for communication differences. Talk therapy does not account for those with processing differences and literal interpretation. Those with social anxiety or situational mutism are unable to book appointments due to the requirement to telephone first. Access barriers and an inflexible system results in neurodivergent clients being further disadvantaged and more likely to not get the help they need. When they don’t engage, the system usually blames them rather than looking within for a system change that could benefit all.
Supporting neurodivergent people, of any age, requires us to urgently grapple with our established clinical practice and beliefs. We, as health and social care professionals (especially occupational therapists and speech and language therapists) have a duty of care to ensure we uphold and promote the human rights, including cultural rights, of everyone who comes under our care. We are duty bound to abide by the standards and code of conduct set by the HCPC in the UK and CORU in Ireland, and our regulatory bodies. As professionals, we possess power and privilege in our positions that we can use to support and advocate for neurodivergent people in ways that allows them to achieve outcomes that align with the Neurodiversity Model – Agency, Autonomy, Authenticity and Acceptance.
While we seek to improve services and support for our neurodivergent clients, let’s not forget that many of our colleagues are neurodivergent and would also benefit from a work environment which values these outcomes for all humans.
This OTalk chat has been put together by a group of occupational therapists and speech and language therapists – some who are neurodivergent themselves.
We know that all professionals want to provide the best support they can for the people in their care – and so by helping to inform those who might be unaware of the need to change our practices, and the injustices and human rights issues that exist, we hope that this discussion will be the start of how we can all change, to be neurodivergent-affirmative in everything we do.
Questions for the chat:
1. What is your understanding of the terms Neurodiversity and Neurodivergent?
2. What is your understanding of the term neuro-affirmative and why is it so important for our practice?
3. What are you already doing to support your neurodivergent clients?
4. What are the barriers to practicing in a neuro-affirmitive manner? Do you have plans to address these?
5. Do you have resources you can share to improve practice?
Information about some of the contributors:
Elaine McGreevy, Speech and Language Therapist
Twitter: @ElaineMcgreevy
Elaine is the Founder Director of Access Communication C.I.C., a community interest company, established in April 2021, which offers pro-neurodiversity Speech and Language Therapy and related services for the direct or indirect benefit of autistic children and young people. In January 2021, Elaine assumed the role of Senior Advisor at the Therapist Neurodiversity Collective; an international collective of licensed and/or credentialed therapists and psychologists with a shared mission in advocating for change in therapy practices, away from behavioural-based interventions to naturalistic, empathetic, respectful therapy practices, which affirm neurodivergence. Elaine has worked predominantly in the NHS in Northern Ireland, until 2021. In a Clinical Lead role, since 2001, Elaine’s work has involved setting up and developing of speech and language therapy services and diagnostic services for autistic children and young people.
Alice Hortop is a senior occupational therapy lecturer at UWE in Bristol. She is openly neurodivergent and facilitates a neurodivergentOT empowerment group for her students with her fellow neurodivergent colleague. She uses her neurodivergency positively in her role both as an expert by experience and role model. Twitter handle @LaughingOT
@OT_Expert – A neurodivergent occupational therapist who passionately wants to help change the understanding and practice of health and social care professionals (and everyone else!) to be neurodivergent affirmative.
Susan Griffiths – @SusanGriffiths5 – Paediatric deaf occupational therapist lead with post grad diploma in Sensory Integration, working with autistic children. Founder of @AbleOTUK.
Niamh Mellerick – @Niamh_Mell – Occupational therapist. Part of the @AslAmIreland team. Occasionally educating as part of the @OTatBrunel London team.
POST CHAT
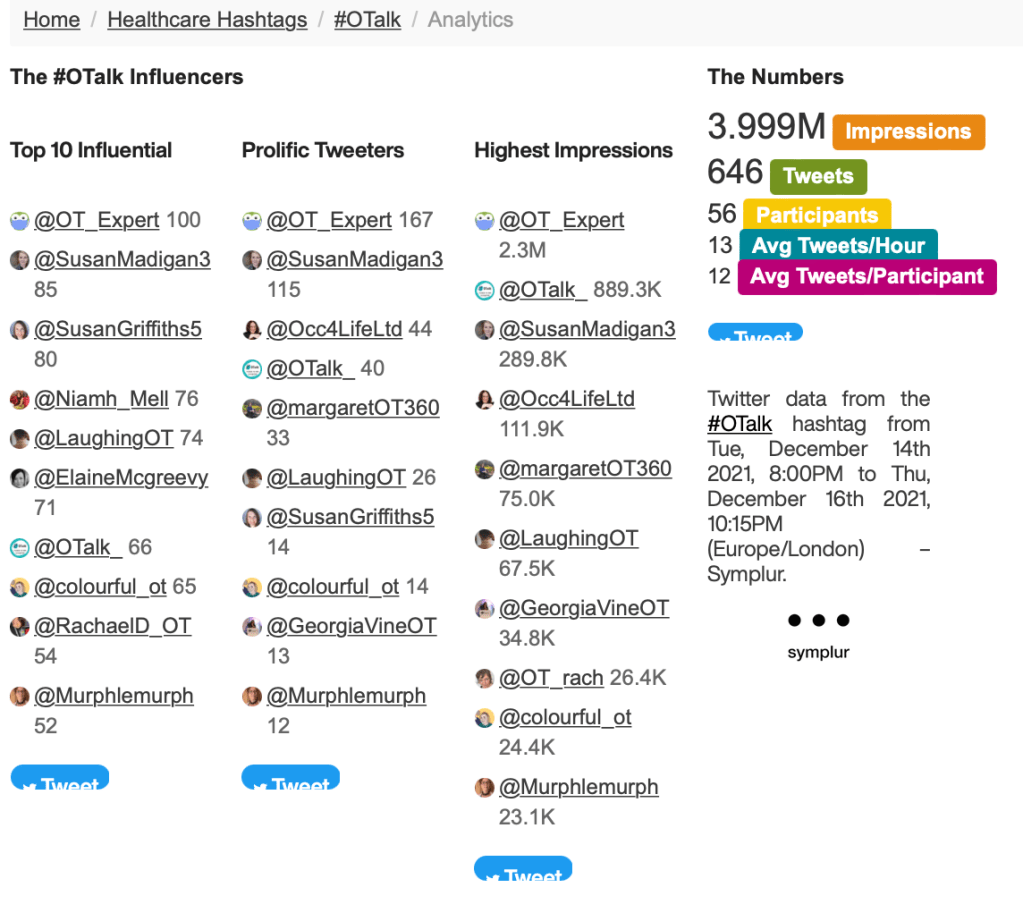
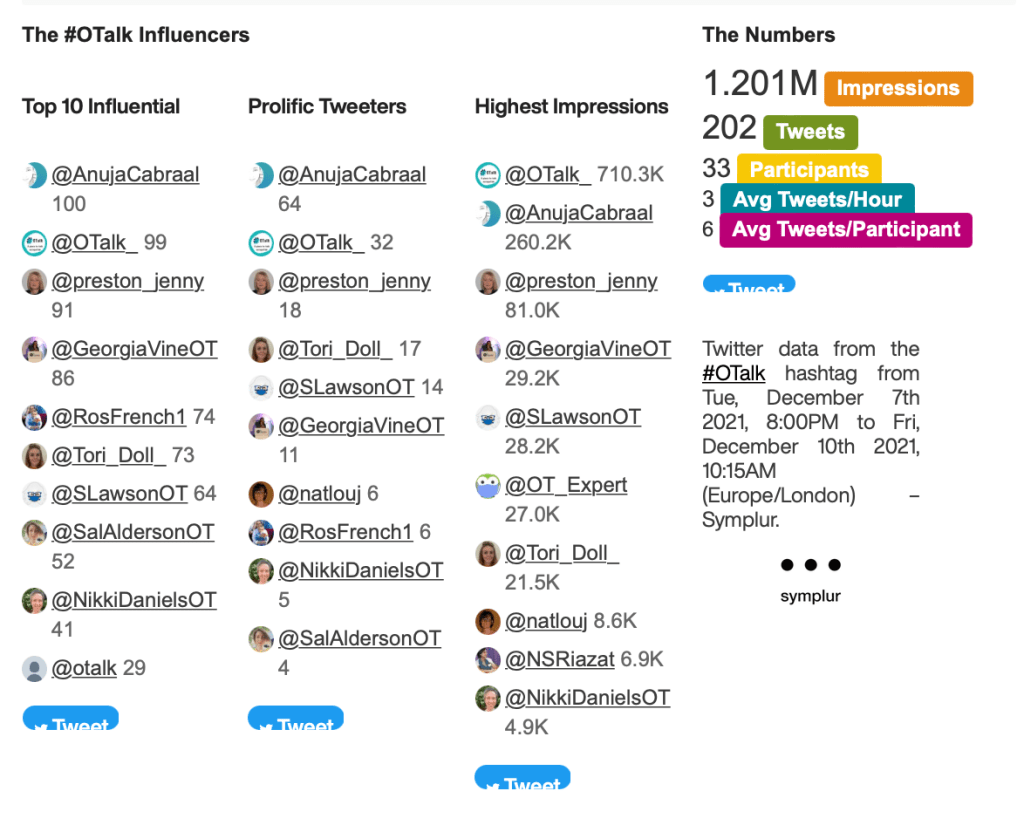
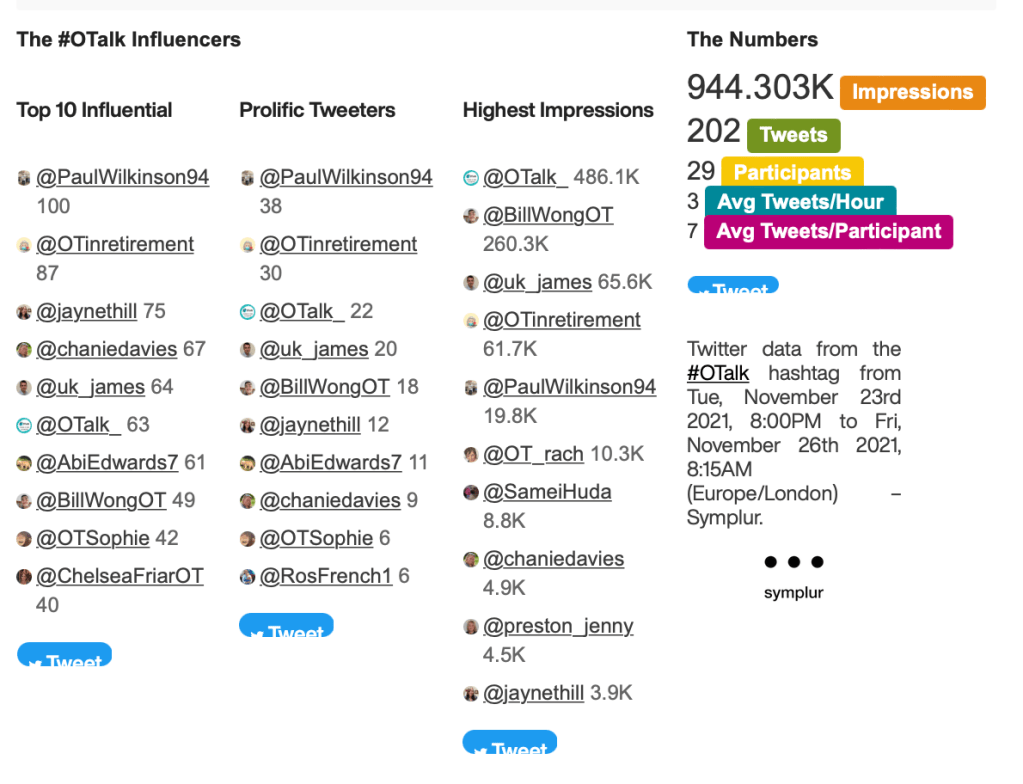
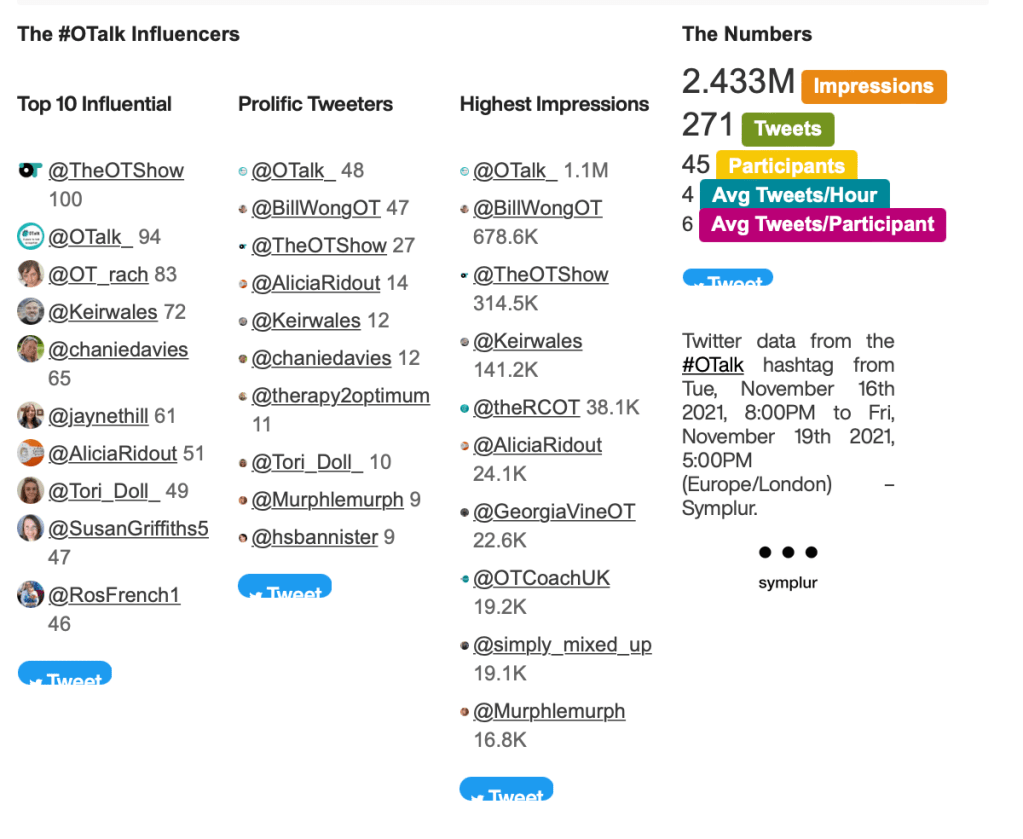
Host: @OT_Expert
Support on OTalk Account: @otrach
Evidence your CPD. If you joined in this chat you can download the below transcript as evidence for your CPD, but remember the HCPC are interested in what you have learnt. So why not complete one of our reflection logs to evidence your learning?
HCPC Standards for CPD.
- Maintain a continuous, up-to-date and accurate record of their CPD activities.
- Demonstrate that their CPD activities are a mixture of learning activities relevant to current or future practice.
- Seek to ensure that their CPD has contributed to the quality of their practice and service delivery.
- Seek to ensure that their CPD benefits the service user.
- Upon request, present a written profile (which must be their own work and supported by evidence) explaining how they have met the Standards for CPD.