As part of the Diabetes Week, I’m facilitating today’s Twitter discussion to talk about whether occupational therapists can help people manage their diabetes. Diabetes Week is around the third week of June from the 12th to the 18th. During this crucial week it raises awareness of the condition, and it gives an opportunity for everyone to gather and support those who are affiliated with Diabetes.
According to Tack et al. (2018) people living diabetes on average, can make up to 180 decisions related to diabetes per day. Good glycaemic control is achieved by the hourly decisions made by those living with diabetes. Whilst having an insulin pump makes monitoring slightly easier, the burdens of managing diabetes are a daily chore for the person living with this condition. “Technological advances like insulin pumps and continuous glucose monitors or flash glucose monitors are relatively good, However, they still require concerted effort. Other things that come with diabetes like counting carbohydrates, decision-making around exercise and its impact on insulin relies on patient input, considering all activities in the day that they anticipate to engage in.
Diabetes management is a demanding task that calls for consistency, order, and stability. To effectively follow the diabetes regimen, self-care is necessary. According to the Diabetes self- management (DSM), self-care is letting diabetics understand and pay attention to their bodies and minds while they are experiencing the effects of diabetes.
This twitter chat aims to determine whether occupational therapists can help people with diabetes manage their condition. There is currently very little evidence to support the role of an occupational therapist, which is why it is important to support patients who live with diabetes.
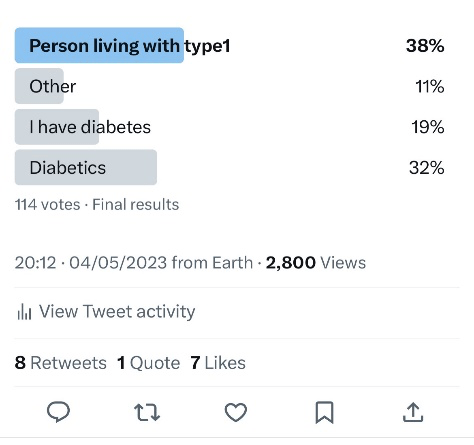
According to a twitter poll on the 4th May, 2023 people with diabetes may address themselves differently to their friends vs when reviewed by health professionals. ( See Poll results) .
What is Diabetes?
Diabetes is a condition caused when a person’s glucose level becomes elevated and becomes high. There are four types of diabetes: Pre-diabetes, Type 1 diabetes, Type 2 diabetes, and gestational diabetes. (WHO, 2016). Five million individuals in the United Kingdom have diabetes, according to Diabetes UK, (2023). In the UK, 4.3 million individuals currently have diabetes diagnosis. We are aware that type 2 diabetes makes up around 90% of diagnoses, followed by type 1 diabetes which equates to about 8%, and the other 2% of diagnoses are for different forms of the disease.
Type One Diabetes occurs when the body fights the cells in the pancreas that produce insulin, and so preventing production of insulin. Everyone needs to have insulin in order to stay alive. Glucose moves around an individual’s blood and enters their cells and gives their bodies energy. This is facilitated by the presence of insulin. When an individual has Type 1 diabetes, their body still breaks down carbohydrates from food and drinks into glucose (sugar). However, when the glucose enters the bloodstream, the lack of insulin means it is unable to enter the body’s cells. Glucose then builds up in your bloodstream (Diabetes UK, 2012).
Type Two Diabetes is a condition when the pancreas cannot work efficiently to make insulin. The role of the pancreas is to distribute insulin, when this does not occur this causes high glucose levels. In Type Two diabetes, the pancreas can become more tired causing the body to produce less insulin. Type 2 can be managed by lifestyle changes like healthy eating, regular exercise and losing weight (Diabetes UK, 2012). Otherwise, alternative treatment such as medications or insulin may be appropriate.
Other types of diabetes include gestational diabetes, a temporary condition in pregnancy where the mother becomes insulin resistant (WHO, 2016), and ‘pre-diabetes’ which places the individual at higher risk of Type 2 Diabetes (American Diabetes Association, 2011).
Diabetes and Occupational Therapy
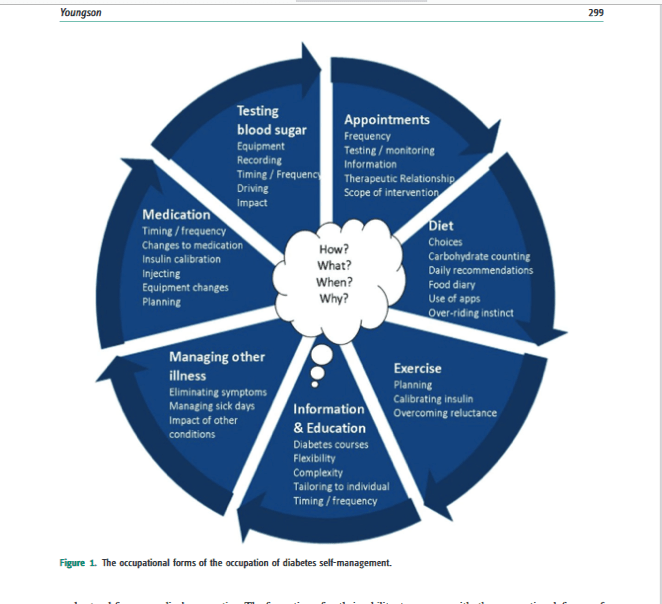
Early studies on OTs and diabetes focuses mostly on the OTs involvement in managing diabetes complications (Hand et al., 2011). The function of OTs in Diabetes Self-Management (DSM), with or without such complications, will be the main topic of this session. By seeing DSM as a profession, it’s becoming clear that the OT can play a major role in enabling and supporting DSM and promoting a fulfilled happy life with diabetes. Exhibited results are presented in Youngson (2019) as a pie chart (p298-300- Please see diagram above). In two additional tables, the results are organised into the MOHO categories of environment, habit, and performance in a format that is simple to understand. For instance, Youngson (2015, 2019) and Pyatak (2011) both point out a gap in earlier research that has neglected to explore the impact of the OT in assisting control of Diabetes in daily life.
This is an under-researched area and the role of the OT in diabetes is sparse. However, the main findings are around complications of diabetes.
Questions
- What are the current roles for occupational therapist in supporting diabetes self – management?
- What occupational therapy intervention could be used to support diabetes self-management?
- What are the views of health professionals and the potential for occupational therapists to support self-management in people with diabetes?
- What does the future of Occupational therapy practice need to support diabetes and OT in practice?
- What could be the role of the occupational therapist in support adults in self-management in relation to mental health and diabetes burn out.?
- What is your takeaway from tonight’s chat? What will you share with others about tonight’s chat?
Reference List:
Diabetes UK (2023) Diabetes Week 2023.Available from :https://www.diabetes.org.uk/diabetes-week [ Accessed 16th April 2023].
Diabetes UK (2023) Number of People living with diabetes in the UK tops 5 million for the first time. Available from: https://www.diabetes.org.uk/about_us/news/number-people-living-diabetes-uk-tops-5-million-first-time [Accessed 16th April 2023].
Hand, C. L., Letts, L. J. and von Zweck, C. M. (2011) ‘An agenda for occupational therapy’s contribution to collaborative chronic disease research’, Canadian Journal of Occupational Therapy, 78(3), pp. 147–155. doi: 10.2182/ciot.2011.78.3.2.
Pyatak, E. (2011) ‘Participation in Occupation and Diabetes Self-Management in Emerging Adulthood’, American Journal of Occupational Therapy, 65(4), pp. 462–469. doi: 10.5014/ajot.2011.001453.
Pyatak, E. et al. (2019) ‘Addressing Diabetes in Primary Care: Hybrid Effectiveness–Implementation Study of Lifestyle Redesign® Occupational Therapy’, American Journal of Occupational Therapy, 73(5), pp. 1–12. doi: 10.5014/ajot.2019.037317.
Tack, C. J. et al. (2018) ‘Glucose Control, Disease Burden, and Educational Gaps in People with Type 1 Diabetes: Exploratory Study of an Integrated Mobile Diabetes App’. doi: 10.2196/diabetes.9531.
Youngson, B. (2019) ‘Understanding diabetes self-management using the Model of Human Occupation’, British Journal of Occupational Therapy, 82(5), pp. 296–305. doi: 10.1177/0308022618820010.