This week Jay Webster will be hosting this is what they have to say to get you thinking about this weeks topic.
Patient and public involvement (PPI) is a term that has been used a lot when talking about working with people but I’m trying to use it less to reduce acronym use and confusion, after all, we’re not talking about insurance or medicine for heartburn.
For this #OTalk, however, due to character restrictions, PPI can be used freely when talking about public involvement
Public involvement means working with people, often called public contributors, rather than doing things to, for or about them (NIHR, 2021). We can involve the public in our occupational therapy practice, for example: consulting with them about service development, getting their input to design patient leaflets and posters or changing the way we offer occupational therapy to certain groups of people; or in research, where members of the public can work alongside researchers to formulate questions, apply for funding, design projects and carry out the research.
The term public includes patients, carers, service-users and representative organisations. Wider stakeholders such as funders and health professionals get involved in different ways and while they have the potential to become patients and are essentially members of the public, their roles are very different when it comes to public involvement.
Other terms for public contributors include patient partners, experts by experience, survivors, patient representatives, co-production advisers, lay contributors and patient leaders.
When talking about involving the public in our practice, I mean at a service level rather than at an individual conversation between therapist and patient. That said, sometimes the best involvement starts from having an early conversation and grows, leading to changes in service provision, but we’re talking about something different to a patient being involved in the decisions around their care (shared decision making – that’s a whole different #OTalk).
This week’s #OTalk is being hosted by @jaywot77 and some of you will know that they are currently undertaking a PhD in public involvement in health and care research. They want to make it clear that nothing that is said in this OTalk will be used in their research, this is purely for interest and to see what people think about involving the public in various ways. Jay is feeding their curiosity not gathering data at this time.
Many people believe that involving the public improves the quality of services (NHS Health Research Authority, 2021) and increases research impact (Brett et al, 2014) and I hope that hosting this #OTalk might help more people see that the people we work with deserve to be much more involved in their care services rather than standing by while we develop services around them. Let’s start with the people we serve and include them in all that we do. Afterall, what we do is for them so we should really be working with them to make occupational services the best that they can be.
OTalk – “Patient and public involvement in research and in practice – how can we get people more involved?”
Q1. Do you think patient and public involvement in occupational therapy practice is important? Why/Why not? #OTalk
Q2. What benefits could involving people in occupational therapy practice or research have?
Q3. Can you think of any disadvantages of involving people in occupational therapy practice or research?
Q4. Have you any thoughts about how to involve people more in your practice such as service development?
Q.5 After this #OTalk, do you think you might consider involving people more in your practice, or research if you’re involved in research?
References
Brett, J., Staniszewska, S., Mockford, C., Herron-Marx, S., Hughes, J., Tysall, C., and Suleman, R.A. (2014) `Systematic review of the impact of patient and public involvement on service users, researchers and communities’, Patient, 7(4), pp. 387-95. DOI: 10.1007/s40271-014-0065-0
NHS Health Research Authority (2021) Public involvement in a pandemic: lessons from the UK COVID-19 public involvement matching service. Available from: https://www.hra.nhs.uk/planning-and-improving-research/best-practice/public-involvement/public-involvement-pandemic-lessons-uk-covid-19-public-involvement-matching-service/
NIHR (2021) Briefing notes for researchers – public involvement in NHS, health and social care research. Available from: https://www.nihr.ac.uk/documents/briefing-notes-for-researchers-public-involvement-in-nhs-health-and-social-care-research/27371
POST CHAT
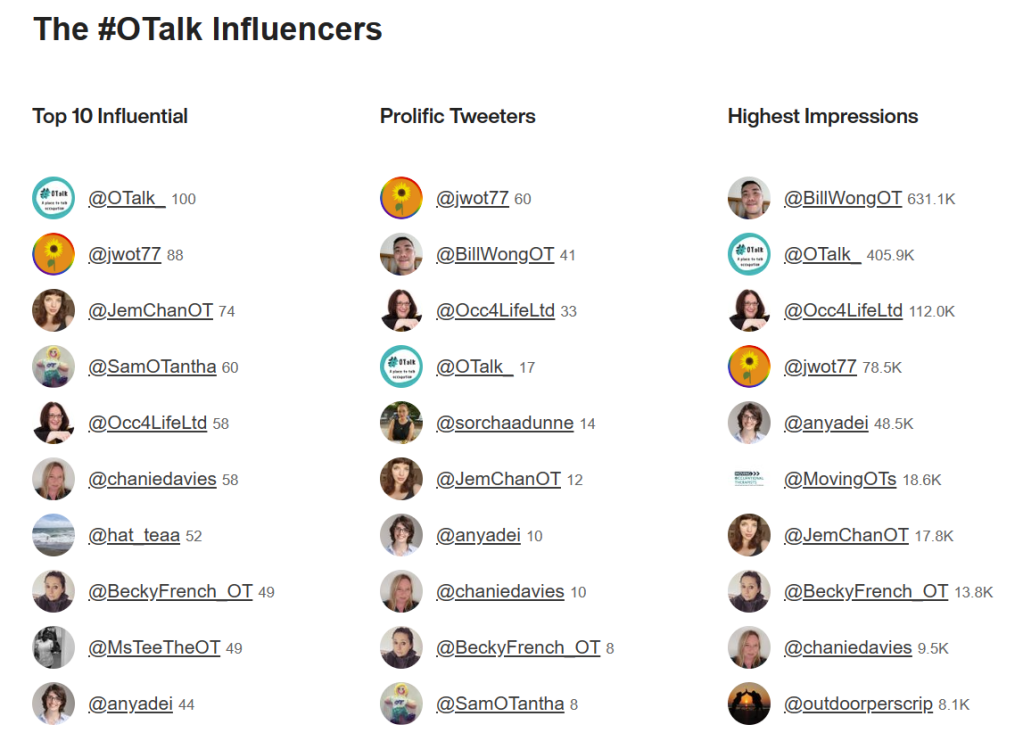
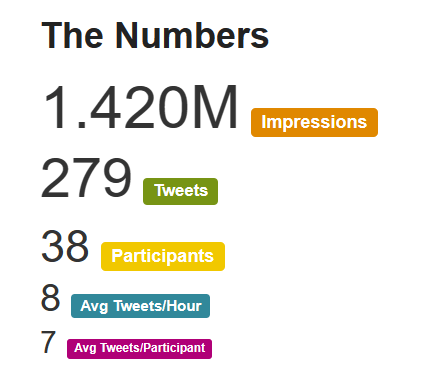
Host: Jay Webster @jwot77
Support on OTalk account: Sam Pywell @smileyfacehalo
Evidence your CPD. If you joined in this chat you can download the below transcript as evidence for your CPD, but remember the HCPC are interested in what you have learnt. So why not complete one of our reflection logs to evidence your learning?
HCPC Standards for CPD.
- Maintain a continuous, up-to-date and accurate record of their CPD activities.
- Demonstrate that their CPD activities are a mixture of learning activities relevant to current or future practice.
- Seek to ensure that their CPD has contributed to the quality of their practice and service delivery.
- Seek to ensure that their CPD benefits the service user.
- Upon request, present a written profile (which must be their own work and supported by evidence) explaining how they have met the Standards for CPD.

1 thought on “OTalk – Tuesday 13th December 2022 8pm – “Patient and public involvement in research and in practice – how can we get people more involved?” hosted by @jwot77”