This week’s chat will be hosted by Tori Wolfendale @Tori_Doll_ here is what she has to say. If you’re new to OTalk find out here how to join in live on twitter every Tuesday 8pm Supported by Rachel
Tori is employed as the Head of Rehabilitation and Recovery Service within a High Secure Forensic mental health service and is currently completing a Professional Doctorate in Health and Social Care – with the focus of her research being on enhancing coproduction within forensic mental health services, promoting the role of Occupational Therapy and how the profession can positively contribute to reducing restrictive interventions and in enhancing the patient “voice” within this to collaboratively identify novel practical solutions or approaches to progressing patients out of the seclusion environment.
What is known regarding seclusion and long-term segregation from contemporary literature:
In the United Kingdom (UK), patients are admitted to secure forensic services because they are deemed to pose a risk of violence to others and are considered a grave risk to members of the public (O’Dowd, 2022). This is linked to having a history of serious violence, risk to self and presenting with challenging behaviour (Holley et al., 2020). In addition to this, many of the individuals detained within secure services will have a complex mental health history or chronic psychiatric disorders and demonstrate a significant level of risk to themselves or others, which requires care and treatment within the secure environment (Puzzo, 2022).
The term ‘long-term segregation’ (LTS) is defined in the Mental Health Act Code of Practice (2015) as a highly restrictive intervention “which is only used when a patient is considered to present with chronically high-risk behaviours or potential of serious harm to other people that cannot be managed in a less restrictive manner”.
Whilst it has been argued that restraint and the use of seclusion and segregation are necessary for maintaining patient and staff safety, Wilson et al., (2017) propose that these approaches continue to be frequently used in contemporary practice. Furthermore, Ezeobela et al., (2014) argues that these practices have negative consequences on all stakeholders, with staff and patients reporting feelings of distress, anxiety, fear and experiencing a loss of identity, resulting in further emotional distress and social isolation. What is known from contemporary literature is the use of seclusion, LTS and restraint has been shown to have adverse effects on the therapeutic milieu, damage to patient and staff relationships and are perceived by staff to be incompatible with caring values that are a core aspect of working within any healthcare environment (Chaung and Huang, 2007). Supplementarily, there is also a growing body of literature that recognises that simply witnessing restraint or the use of restrictive interventions can have negative psychological implications for mental health patients and staff (Wilson et al., 2007; Holmes et al., 2015; Price et al., 2017). However, with austerity, underfunding, the current impact of the global pandemic and the associated staffing and resource deficits, the exponential growth in segregation across secure mental health services is becoming increasingly problematic (Chandley, 2022).
Where does Occupational Therapy fit into this?
One of the key political drivers within forensic services specifically, is that care providers must implement measures to enhance the experience, independent living skills and quality of life for patients with long-term conditions by ensuring that their care consists of a minimum of 25 hours of meaningful activity each week. This can pose a challenge for patients in long-term segregation as by definition, the patient is “specifically placed alone in a locked room for a period at any time of the day or night for the protection of the patient, staff or others from serious harm” (Newton-Howes, 2013, p. 422), which can significantly reduce their opportunities to engage in activities outside of their room. Additionally, the National Institute for Clinical Excellence (NICE) guidelines argues for the least restrictive measures to be used at all times and that the use of seclusion should be a last resort (NICE, 2021). The Occupational Therapy profession contributes to this process by prescribing meaningful activity as a therapeutic tool, based on the individual’s preferences and needs. Ozkan et al., (2018) remind us that individuals who need forensic rehabilitation experience considerable participation limitations when engaging in meaningful activities, causing occupational deprivation, a sense of hopelessness and these limitations can contribute to a deterioration in mental health and wellbeing. Furthermore, the aim of Occupational Therapy in this environment is to enable the individual to experience occupational enrichment and achieve optimal functioning through engaging in meaningful activity to mitigate risk (Ozkan et al., 2018).
Questions for you to consider in preparation for the #OTalk community:
- What is your experience of working with patients who require the use of seclusion or long-term segregation?
- How do you remain client-centred throughout this process?
- What are the challenges or barriers to working effectively with patients who require the use of seclusion or long-term segregation? How does this influence your clinical practice? How do you overcome these? Please share any key learning outcomes.
- What are the positive factors when working with patients who require the use of seclusion or long-term segregation? Please share any key learning outcomes.
- What best practices have you identified through your experience?
- What evidence-based practice do you use to underpin your practice when working with patients who require the use of seclusion or long-term segregation?
- What models of practice do you use to underpin your clinical practice when working with patients who require the use of seclusion or long-term segregation? How does this influence your practice?
- Has COVID19 had any influence on your practice when working with patients who require the use of seclusion or long-term segregation?
- Finally … please share one specific success story – let’s use this as an opportunity to really showcase with the wider Twitter Community the fantastic work that Occupational Therapist’s complete with this complex patient group! What was this? Why was this successful? What was the impact?
POST CHAT
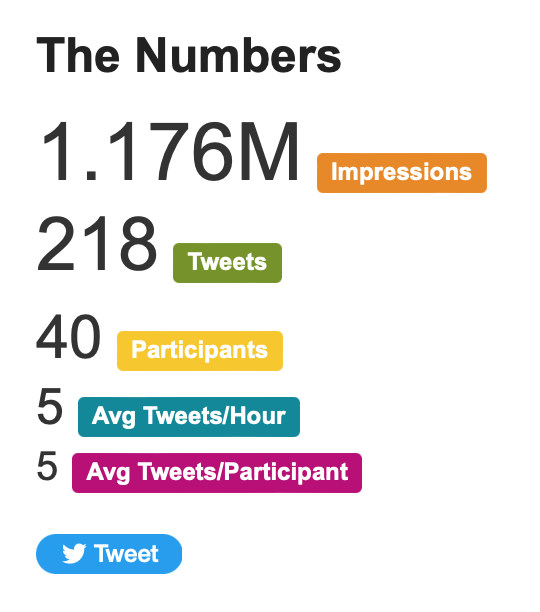
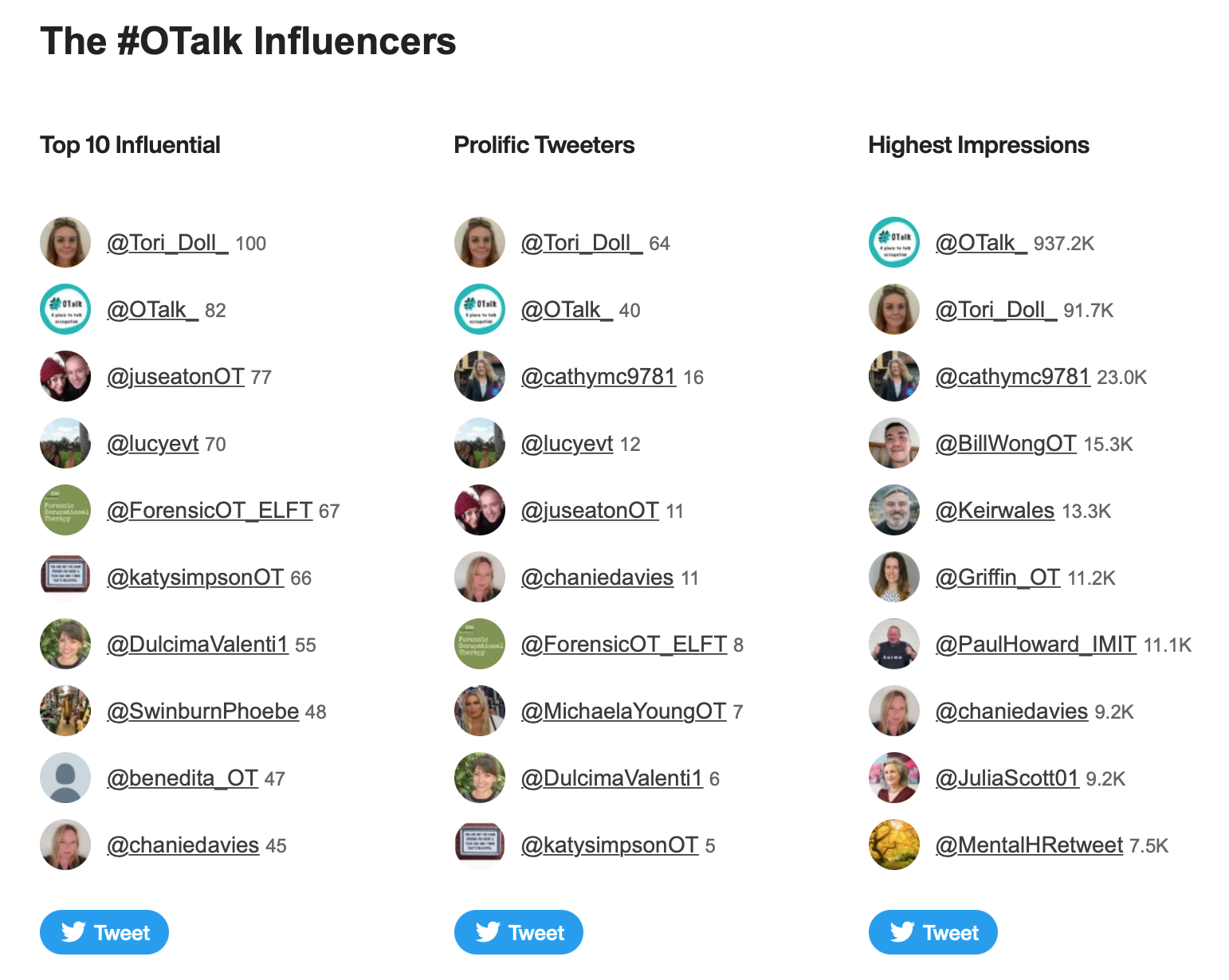
Host: Tori Wolfendale @Tori_Doll_
Support on OTalk Account: Rachel @OT_rach
Evidence your CPD. If you joined in this chat you can download the below transcript as evidence for your CPD, but remember the HCPC are interested in what you have learnt. So why not complete one of our reflection logs to evidence your learning?
HCPC Standards for CPD.
- Maintain a continuous, up-to-date and accurate record of their CPD activities.
- Demonstrate that their CPD activities are a mixture of learning activities relevant to current or future practice.
- Seek to ensure that their CPD has contributed to the quality of their practice and service delivery.
- Seek to ensure that their CPD benefits the service user.
- Upon request, present a written profile (which must be their own work and supported by evidence) explaining how they have met the Standards for CPD.